Get Well Clinic makes virtual care accessible
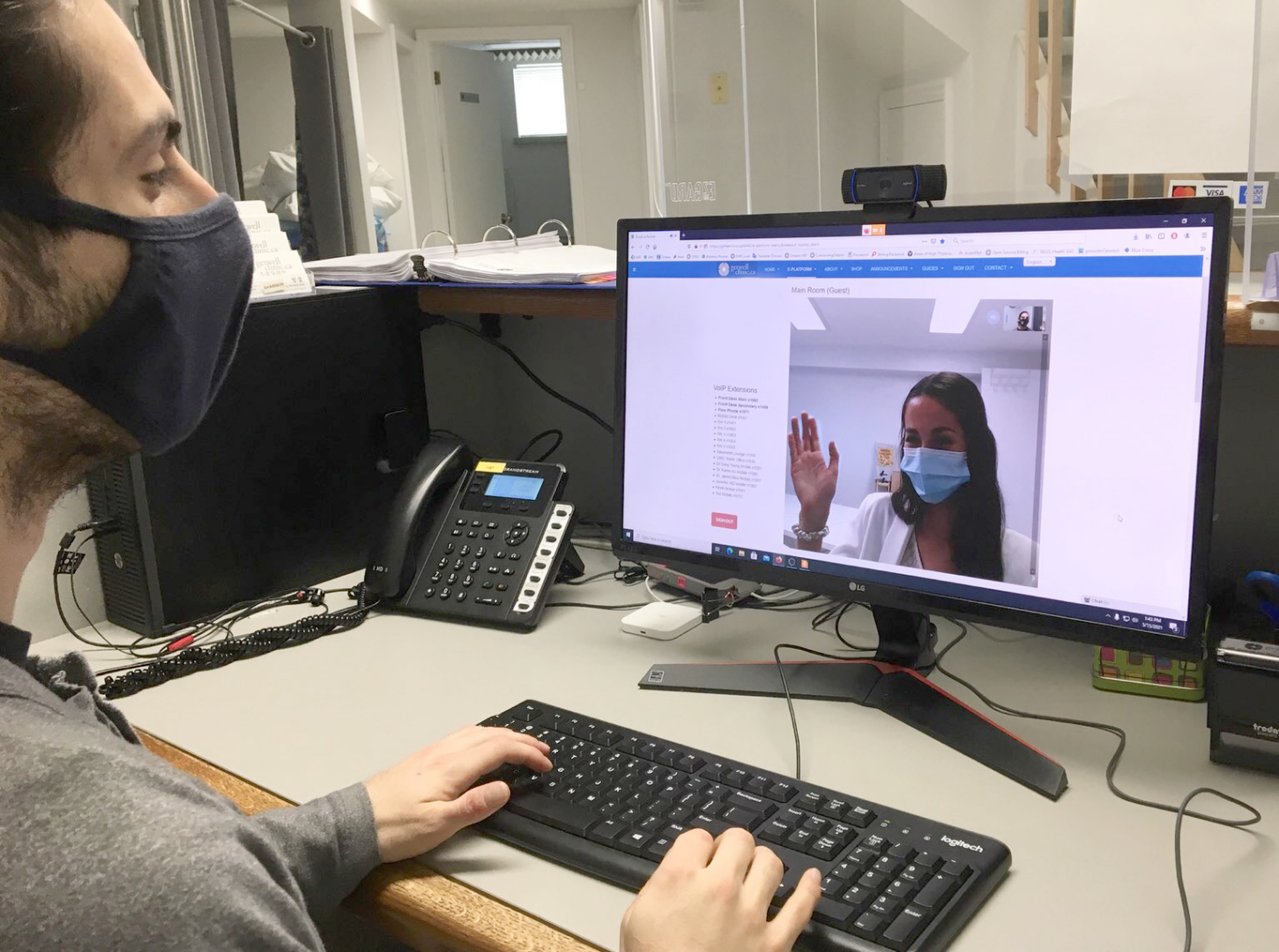
Since the start of the COVID-19 pandemic, virtual care has been supplementing and replacing traditional in-person clinical visits. It has become a seamless, convenient way to directly connect patients with health care providers and community support services and allows people to speak with their doctor from the comfort of their homes.
Virtual care is still relatively new in Ontario’s health system and to be successful virtual services need to be easy and accessible for all patients and caregivers who could benefit.
Medical researchers at North York General Hospital (NYGH) introduced technical support and chat helpdesk capabilities to increase patient access to physicians and other professionals through video conferencing. At the onset of the pandemic, Get Well Clinic, an interdisciplinary clinic partnering with NYGH, that provides medical, health and wellness care, rapidly pivoted to a hybrid virtual and in-person care model by implementing an open-source electronic platform and expanding their team to include technical support and offer live chat features for their patients.
“We reached an extraordinary level of video-enabled appointments—even reaching 90 percent at one point,” says Dr. Kevin Lai, Medical Director of the clinic. “By expanding our team of professionals and providing technical support to our patients, we were able to minimize disruptions to health care access.”
Dr. Lai recently conducted a quality improvement study to evaluate the effectiveness of measures put in place to respond to the pandemic. These measures included introducing a new video conferencing platform, staff restructuring, employee training and establishing a new volunteer program.
The study found that although there was a reduction in physician-patient encounters at the beginning of the pandemic, the numbers recovered and steadily increased as patients accessed new video appointments.
“Considering that the vast majority of patient-doctor encounters in Ontario during COVID shifted to telephone, we are very happy to be able to provide video-enabled services to our patients,” says Lai.
“Virtual appointments are becoming more and more accepted as a way of delivering patient care,” says Dr. Karen Tu, Research Scientist and Family Medicine Research Lead at NYGH and senior author for the study. “We wanted to understand how this shift to virtual care impacted patients from low-income communities, and whether widely adopted virtual appointments have worsened disparities in access to primary care.”
Researchers looked at electronic medical record (EMR) patient data from the University of Toronto Practice Based-Research Network (UTOPIAN) and found that virtual care was accessed by patients from across socioeconomic groups.
Telephone and video appointments may have in fact helped ease some barriers to accessing health care, such as the need to take time off work, arrange childcare or commute to appointments.
“Looking at EMR research data can make an enormous difference in understanding what happens to patients in the community,” explains Dr. Michelle Greiver, Gordon F. Cheesbrough Research Chair in Family and Community Medicine at NYGH. “It’s important to know that groups of people are not being disadvantaged as we consider virtual care and what’s best for each patient.”